Volume 29, Number 10—October 2023
Dispatch
Mpox in Children and Adolescents during Multicountry Outbreak, 2022–2023
Abstract
The 2022–2023 mpox outbreak predominantly affected adult men; 1.3% of reported cases were in children and adolescents <18 years of age. Analysis of global surveillance data showed 1 hospital intensive care unit admission and 0 deaths in that age group. Transmission routes and clinical manifestations varied across age subgroups.
Mpox is a zoonotic disease caused by monkeypox virus (MPXV) and previously found primarily in forested areas of Central and West Africa (1,2). In May 2022, a multicountry outbreak of mpox emerged; as of May 2023, there were >87,500 cases and 141 deaths reported from 111 World Health Organization (WHO) member countries (3). Globally 1.3% of reported cases during the outbreak have been in children and adolescents <18 years of age (3). During 1970–2021, mpox cases in Central Africa were predominately (54%–90%) reported in children (4–6), and children experienced more severe disease and adverse outcomes than adults (6,7).
After the first cases of mpox from countries without a history of the disease were reported to WHO in May 2022, a global surveillance system was established to collect aggregated data on probable and confirmed cases, as well as detailed case-based information on demographics, medical history, clinical manifestations, exposure factors, and testing (8). We describe epidemiologic and clinical characteristics of mpox in case-patients <18 years of age using surveillance data reported by all WHO regions during January 1, 2022–May 22, 2023 (https://www.who.int/publications/i/item/WHO-MPX-Surveillance-2022.4).
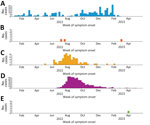
During the study period, 1.3% (1,118/84,614) of confirmed mpox cases globally were in patients <18 years of age. Most (61.8%, 691) were from the WHO Region of the Americas, followed by the African Region (30.3%, 339), the European Region (7.5%, 84), the Eastern Mediterranean Region, (<1%, 3), and the Western Pacific Region (<1%, 1) (Figure 1). No cases in patients <18 years of age were reported from the South-East Asia Region. Countries in the African Region reported mpox cases before the global outbreak (Figure 1), whereas reports of mpox cases in Europe and in the Americas began in May 2022 and peaked in July–August 2022. In Europe and the Americas, the epidemic curve of case-patients <18 years of age closely mimics the overall regional curves (3). The global percentage of case-patients <18 years of age has consistently remained low (0%–3%). By May 2023, overall case counts were low across all regions; the Americas, the Eastern Mediterranean Region, and the Western Pacific Region reported sporadic case-patients <18 years of age. Among the 1,102 case-patients <18 years with available information, 59.3% (654) were male and 40.7% (448) female (Appendix Figure).
MPXV has 2 distinct clades, I and II (9). Virus clade information was not available for most cases and was assumed on the basis of the reporting country or subnational area and circulating clades in 2022, as reported by countries on GISAID (https://www.gisaid.org) or Nextstrain (https://nextstrain.org), in published literature, or to WHO. Of the 297 cases of mpox from countries reporting clade I, all age groups had a similar sex distribution (Appendix Figure, panel A). Of the 805 cases of mpox from countries reporting clade II, there were more male than female case-patients (269 vs. 104) among those 13–17 years of age. (For cases from Cameroon, 4 from eastern Cameroon are included in the clade I distribution, 1 from western Cameroon is included in the clade II distribution, and 1 for which we had no detailed geographic information was excluded.) Of case-patients with available hospitalization data, 47/335 (14.0%) were hospitalized and 1 was admitted to the intensive care unit; none was reported to have died.
Data on self-reported sexual behavior were limited for mpox case-patients <18 years of age. However, 37/166 (22.3%) of case-patients 13–17 years of age self-identified as men who have sex with men (MSM) (Table 1). Eleven cases involved persons living with HIV, 1 of whom was immunosuppressed. Another 6 case-patients reported immunosuppression, as defined by their care providers, that was caused by undisclosed medical conditions. Overall, 67/293 (22.9%) of cases with information provided had a stated epidemiologic link to a known mpox case.
Case-patients 0–12 years of age were exposed to MPXV mainly through physical person-to-person contact (excluding sexual contact) or contact with fomites, whereas exposure through sexual encounter was exclusively reported by those 13–17 years of age (Figure 2). Among the older group, some of whom self-identified as MSM, sexual transmission may explain the unequal sex distribution of clade II cases (Appendix Figure, panel B). The type of transmission was reported as other in 32/118 (27.1%) of cases, without additional information.
Among cases with data, 472/542 (87.1%) experienced symptoms (Table 2). We excluded from analysis cases reported to be symptomatic but without any specific symptom. The presence of any rash, which consisted of >1 rash symptoms (on the body, oral, genital, or unknown location), was the predominant symptom for all age groups (325/542, 60%); genital rash was present in 54/229 (23.6%) of case-patients 13–17 years of age and 19/313 (6.1%) of those <13 years of age (p<0.00001). Among case-patients 13–17 years of age who reported being infected through sexual contact, genital rash was present in 15/34 (44.1%). Genital rash may be indicative of the transmission route of mpox but can also be present when transmission has not occurred through sexual contact. After rash, the most reported symptoms were fever (270/542, 49.8%) and headache (158/542, 29.2%). Lymphadenopathy has been reported as a common mpox symptom (1,6); it was reported in 60/542 (11.1%) of cases in our study.
During this outbreak, countries with high caseloads reported most of the case-patients <18 years of age, however, the percentage of pediatric and adolescent patients in those countries was lower than that for adults. The percentage of patients <18 years of age was lower than had been feared early in the outbreak, amid concerns that the epidemic could shift from primarily affecting MSM to a more generalized epidemic spread, including among school-age children. Epidemiologic and clinical characteristics were similar for the age groups 0–4 and 5–12 years, whereas case-patients 13–17 years of age, who are more likely to be sexually active, commonly reported MSM sexual behavior, exposure through sexual contact, and having more genital lesions.
Studies from the Netherlands (10), Spain (11), England (12), and the United States (13,14) have described MPXV infection among children and adolescents during this outbreak. Consistent with our findings, most cases in those studies reported no intensive care unit admissions or deaths; WHO is aware of the death of an infant from mpox clade I for which data are not available (3). Our results differ from historical reports of mpox in children, in which they have been described as at higher risk for adverse events and death related to disease (15). A previous study using the same surveillance data found higher odds of hospitalization for children <5 years of age than for those 15–45 years of age (8). The lower observed severity in children and adolescents in this outbreak than for previous outbreaks may be caused by a combination of increased ascertainment of mild cases, differing access to healthcare between settings, differing health status of the host populations, and lower virulence of clade IIb MPXV; clade I MPXV infection has been reported to be associated with higher severity than clade II (1).
Our study is based on surveillance data and likely underestimates the true number of case-patients <18 years of age, particularly in Africa (8). Disease severity may be underestimated because countries may not have updated case outcomes if hospitalization or death was delayed. Finally, data completeness varied among regions and countries; thus, our results may not be representative of each setting.
This study highlights the need for thorough epidemiologic investigation of mpox in children and adolescents. Clinicians should consider mpox as a possible diagnosis in these age groups when they have indicative symptoms, even with no known epidemiologic link to another case.
Dr. Hoxha is an infectious disease epidemiologist working for WHO Geneva, with special interest in surveillance systems, outbreak investigation, emergency response and epidemiological methods for public health. Mr. Kerr is a data analyst with CPC Analytics supporting the WHO Hub for Pandemic and Epidemic Intelligence in Berlin. His interests include disease modeling, monitoring and evaluation of global health surveillance, and global health disparities.
Acknowledgments
We thank all WHO Member States and their health workers for their engagement and detailed reporting of case-based information to WHO and other regional institutions, in line with temporary recommendations issued by the WHO Director-General under the Public Health Emergency of International Concern within the framework of the International Health Regulations (IHR 2005). Reporting to WHO was made possible through a global collaborative effort involving healthcare professionals, epidemiologists, and public health workers from across the world, to whom we are deeply grateful. For the WHO European Region, we used data reported by countries to ECDC and WHO through The European Surveillance System (TESSy; https://www.ecdc.europa.eu/en/publications-data/european-surveillance-system-tessy).
This work was supported by the World Health Organization contingency fund for emergencies.
References
- Gessain A, Nakoune E, Yazdanpanah Y. Monkeypox. 2022. 387:1783–93. https://www.nejm.org/doi/full/10.1056/NEJMra2208860
- World Health Organization. Epidemiology of human monkeypox (mpox)— worldwide, 2018–2021. 2023 [cited 2023 Mar 23]. https://apps.who.int/iris/handle/10665/365630
- World Health Organization. 2022–23 mpox (monkeypox) outbreak: global trends. 2023 [cited 2023 May 24]. https://worldhealthorg.shinyapps.io/mpx_global
- Besombes C, Mbrenga F, Schaeffer L, Malaka C, Gonofio E, Landier J, et al. National monkeypox surveillance, Central African Republic, 2001–2021. Emerg Infect Dis. 2022;28:2435–45. DOIPubMedGoogle Scholar
- Lourie B, Bingham PG, Evans HH, Foster SO, Nakano JH, Herrmann KL. Human infection with monkeypox virus: laboratory investigation of six cases in West Africa. Bull World Health Organ. 1972;46:633–9.PubMedGoogle Scholar
- Ježek Z, Szczeniowski M, Paluku KM, Mutombo M. Human monkeypox: clinical features of 282 patients. J Infect Dis. 1987;156:293–8. DOIPubMedGoogle Scholar
- Jezek Z, Marennikova SS, Mutumbo M, Nakano JH, Paluku KM, Szczeniowski M. Human monkeypox: a study of 2,510 contacts of 214 patients. J Infect Dis. 1986;154:551–5. DOIPubMedGoogle Scholar
- Laurenson-Schafer H, Sklenovská N, Hoxha A, Kerr SM, Ndumbi P, Fitzner J, et al.; WHO mpox Surveillance and Analytics team. Description of the first global outbreak of mpox: an analysis of global surveillance data. Lancet Glob Health. 2023;11:e1012–23. DOIPubMedGoogle Scholar
- Ulaeto D, Agafonov A, Burchfield J, Carter L, Happi C, Jakob R, et al. New nomenclature for mpox (monkeypox) and monkeypox virus clades. Lancet Infect Dis. 2023;23:273–5. DOIPubMedGoogle Scholar
- Tutu van Furth AM, van der Kuip M, van Els AL, Fievez LCR, van Rijckevorsel GGC, van den Ouden A, et al. Paediatric monkeypox patient with unknown source of infection, the Netherlands, June 2022. Euro Surveill. 2022;27:
2200552 . DOIPubMedGoogle Scholar - Aguilera-Alonso D, Alonso-Cadenas JA, Roguera-Sopena M, Lorusso N, Miguel LGS, Calvo C. Monkeypox virus infections in children in Spain during the first months of the 2022 outbreak. Lancet Child Adolesc Health. 2022;6:e22–3. DOIPubMedGoogle Scholar
- Ramnarayan P, Mitting R, Whittaker E, Marcolin M, O’Regan C, Sinha R, et al.; NHS England High Consequence Infectious Diseases (Airborne) Network. Neonatal Monkeypox Virus Infection. N Engl J Med. 2022;387:1618–20. DOIPubMedGoogle Scholar
- Saunders KE, Van Horn AN, Medlin HK, Carpenter A, Lee PA, Gutierrez L, et al. Monkeypox in a young infant—Florida, 2022. MMWR Morb Mortal Wkly Rep. 2022;71:1220–1. DOIPubMedGoogle Scholar
- Hennessee I, Shelus V, McArdle CE, Wolf M, Schatzman S, Carpenter A, et al.; California Department of Public Health Monkeypox Pediatric Working Group; CDC Monkeypox Pediatric Working Group. CDC Monkeypox Pediatric Working Group. Epidemiologic and clinical features of children and adolescents aged <18 years with monkeypox—United States, May 17–September 24, 2022. MMWR Morb Mortal Wkly Rep. 2022;71:1407–11. DOIPubMedGoogle Scholar
- Bunge EM, Hoet B, Chen L, Lienert F, Weidenthaler H, Baer LR, et al. The changing epidemiology of human monkeypox-A potential threat? A systematic review. PLoS Negl Trop Dis. 2022;16:
e0010141 . DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: August 30, 2023
1These first authors contributed equally to this article.
Table of Contents – Volume 29, Number 10—October 2023
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Ana Hoxha, World Health Organization, Avenue Appia 20, 1211 Geneva, Switzerland
Top