Volume 15, Number 8—August 2009
Dispatch
Predictors of Death after Severe Streptococcus pyogenes Infection
Abstract
An evaluation of the relative importance of host and pathogen factors on the survival rate of patients with invasive Streptococcus pyogenes infection found a number of clinical and demographic factors to be associated with risk for death. Some evidence suggested a seasonal pattern to patient survival rate.
Infectious diseases caused by Streptococcus pyogenes are among the most acutely life threatening. Although invasive S. pyogenes infections are uncommon (3 per 100,000 population annually in the United States, United Kingdom, and Australia) (1–3), the case-fatality rate is high relative to many other infections (1,3,4). Identification of specific host and pathogen characteristics with poor survival rate in patients who have these infections could help identify potential pathogenic mechanisms for further research at a cellular level, potentially resulting in identification of novel therapeutic targets.
As part of a European study of severe S. pyogenes infections, the United Kingdom undertook enhanced surveillance during 2003–2004 (2,5,6). Case-patients were defined as persons with S. pyogenes isolated from a sterile site or from a nonsterile site if the patient had pneumonia, necrotizing fasciitis, puerperal sepsis, meningitis, septic arthritis, or if streptococcal toxic shock syndrome (STSS) developed (7). Methods are reported elsewhere (2,8).
To identify patient outcome, data from England and Wales were linked to death registrations obtained from the Office for National Statistics by using probabilistic methods (9). Deaths were identified that occurred up to 30 days after diagnosis of infection; time between diagnosis and death was measured from the date the culture-positive specimen was taken.
Data were analyzed by using STATA statistical software version 8.2 (Stata Corporation, College Station, TX, USA). A nonproportional test for equality of survivor function (Peto-Peto-Prentice) was used to assess differences between subgroups, with Cox proportional hazards regression used for multivariable analysis.
Of the 3,566 case-patients with severe S. pyogenes infection, 3,422 (96%) had sufficient identifiers to be linked to death registrations and were used for all further analyses. Overall, 698 (20%) case-patients died within 30 days after collection of culture-positive specimens. Risk for death was highest within 1 day after specimen collection (11% [375] extending to 16% [559]) for the first 7 days, beyond which risk for death dropped substantially.
Analysis of the certified cause of death identified an infectious underlying cause in 280 (50%) deaths occurring from any International Classification of Diseases, 10th Revision, condition classification within 7 days. S. pyogenes infection was specified as the cause of death in 5 of these (Table).
Age strongly influenced survival rate; oldest patients had the poorest survival rate-(p<0.001; Figure 1). Most deaths in patients <45 years of age (73/104 [70%]) occurred within the first 2 days, whereas deaths in older age groups were more dispersed over time. Other patient factors were independently associated with risk for death ( Appendix Table). Of patients without any identified concurrent illnesses, 87/518 (17%) died within 7 days.
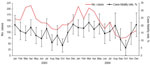
Case-fatality rates paralleled seasonal incidence (Appendix Figure), and were highest from December to April (17%–21%), gradually falling through the summer to their lowest point in October (6%). After adjustment for other significant factors, patients whose infection was diagnosed in October were 82% less likely to die than were those whose infection was diagnosed in January.
Patients identified with necrotizing fasciitis had the highest risk for death within 7 days (34%), >2 times higher than patients with other clinical manifestations, after adjustment for other significant factors. Patients who reported gastrointestinal symptoms were 2 times as likely as those who did not to die within the first 7 days (p = 0.02). Only 9/76 (12%) patients who had gastrointestinal symptoms met the case definition for STSS. Cellulitis, the most common clinical symptom, was associated with more deaths (130/438 [30%] patients) than was any other condition. Survival probability in the 30 days after a culture-positive specimen was significantly reduced among patients in whom STSS developed (p<0.001; Figure 2); 47/178 (26%) of these patients died within a day of specimen collection.
Risk for death varied according to the emm/M-type responsible for the infection. The highest risk was associated with emm/M3 (33%) or emm/M1 (28%), with emm/M3 being borderline significant after adjustment for other significant factors.
This analysis highlighted the scale and rapidity of deaths in patients with severe S. pyogenes infection, reemphasizing the importance of early recognition of invasive disease and prompt initiation of antimicrobial drug and supportive therapy. A number of factors conferred a heightened risk for death, which other studies also have found: increasing age, diagnosis of necrotizing fasciitis or pneumonia, and underlying malignancy (1,10,11). Although necrotizing fasciitis carried the highest risk for all-cause mortality, it is a relatively rare condition, accounting for only 10% of all deaths, compared with the more common and typically less severe cellulitis (30% of deaths). Some evidence indicated that emm/M3 was more commonly associated with death than were other emm/M-types, also found elsewhere (1,11). Development of STSS was a strong predictor of poor outcome, although whether this syndrome is independently related to death is unclear, given that several of its constituent markers effectively denote the progressive failure of organ systems. For this reason, STSS was not included in the multivariable analysis. Notably, patients with gastrointestinal symptoms had a poorer outcome than others; presumably this is a sign of overwhelming sepsis possibly linked to toxin production. Although relatively uncommon (3% of case-patients), gastrointestinal symptoms clearly are of diagnostic importance and should be included in the severity assessment of patients with other signs and symptoms of S. pyogenes infection.
An intriguing and novel finding from this analysis is that risk for death mirrors seasonal changes in incidence (highest in the winter/spring months and falling substantially to a nadir in October). An unadjusted-for confounder could explain this pattern, such as a preceding viral infection, but no candidates with a suitable seasonal pattern are apparent. Although emm/M-type was included in the model, differences could exist in the circulation of specific subtypes with particular virulence profiles throughout the year, again not accounted for in this analysis. Seasonal differences in case-fatality rates may yield some important clues about the drivers behind the seasonal incidence pattern of S. pyogenes infections. An explanation centered wholly around transmission dynamics seems less favored because it would not explain the changing risk for death. An immunologically focused explanation would fit better because it could explain both the changing incidence rate and the changing case-fatality rate. The length of daylight in a given day can affect the production of vitamin D and melatonin. Both vitamin D and melatonin are known to impact immune function (12–14). Although neither appear to be consistent with an autumnal boost to host immunity, if the beneficial effect of vitamin D production during the summer has a cumulative maximal impact in the autumn (15), then this theory could offer an explanation.
Because S. pyogenes is a largely sporadic infection occurring diffusely throughout the population, opportunities for control of severe infections remain limited. The 26 serotypes included in a multivalent vaccine currently under phase II clinical trials represent 67% of all isolates collected in this study, and 80% of all deaths occurring within 7 days after diagnosis (16). The impact of any vaccine will clearly depend on many factors, with the possibility of serotype replacement undermining any such efforts. The challenge to provide a lasting control measure for these devastating infections will continue long into the future.
Dr Lamagni is an epidemiologist working at the Centre for Infections within the Health Protection Agency, London, UK. Her research interests include the epidemiology of streptococcal and fungal infections and of death after infection.
Acknowledgments
We thank the microbiology laboratories across the country for their considerable efforts in reporting cases and referring isolates. We also thank Asha Tanna, Michaela Emery, and Chenchal Dhami for their expert processing of isolates in the Streptococcus and Diphtheria Reference Unit, and the Health Protection Agency Group A Streptococcal Working Group for their efforts in drafting recommendations on the management of community cases of invasive group A streptococcal disease. We thank Neelam Alhaddad for her design of the study database, Jeffrey Dennis for his assistance in analyzing International Classification of Diseases, 10th Revision, codes, George Kafatos for his statistical advice, and the additional members of the Health Protection Agency and Office for National Statistics Steering Group for the Data Linkage Program.
The Strep-EURO project was funded by the European Union Fifth Framework Research Programme (QLK2.CT.2002.01398).
References
- O’Loughlin RE, Roberson A, Cieslak PR, Lynfield R, Gershman K, Craig A, The epidemiology of invasive group A streptococcal infection and potential vaccine implications: United States, 2000–2004. Clin Infect Dis. 2007;45:853–62. DOIPubMedGoogle Scholar
- Lamagni TL, Neal S, Keshishian C, Alhaddad N, George R, Duckworth G, Severe Streptococcus pyogenes infections, United Kingdom, 2003–2004. Emerg Infect Dis. 2008;14:202–9. DOIPubMedGoogle Scholar
- O’Grady KA, Kelpie L, Andrews RM, Curtis N, Nolan TM, Selvaraj G, The epidemiology of invasive group A streptococcal disease in Victoria, Australia. Med J Aust. 2007;186:565–9.PubMedGoogle Scholar
- Tyrrell GJ, Lovgren M, Kress B, Grimsrud K. Invasive group A streptococcal disease in Alberta, Canada (2000 to 2002). J Clin Microbiol. 2005;43:1678–83. DOIPubMedGoogle Scholar
- Public Health Laboratory Service. Enhanced surveillance of invasive group A streptococcal infections. Commun Dis Rep CDR Wkly. 2002;12 [cited 2009 Jun 9]. Available from http://www.hpa.org.uk/cdr/archives/2002/cdr5102.pdf
- Lamagni TL, Darenberg J, Luca-Harari B, Siljander T, Efstratiou A, Henriques-Normark B, Epidemiology of severe Streptococcus pyogenes disease in Europe. J Clin Microbiol. 2008;46:2359–67. DOIPubMedGoogle Scholar
- The Working Group on Severe Streptococcal Infections. Defining the group A streptococcal toxic shock syndrome. Rationale and consensus definitions. JAMA. 1993;269:390–1. DOIPubMedGoogle Scholar
- Neal S, Beall B, Ekelund K, Henriques-Normark B, Jasir A, Johnson D, International quality assurance study for characterization of Streptococcus pyogenes. J Clin Microbiol. 2007;45:1175–9. DOIPubMedGoogle Scholar
- Potz N, Powell D, Pebody R, Lamagni T, Bridger D, Duckworth G. Development of a method to link infection and mortality data. Presented at: Health Protection Agency Annual Conference; 2006 Sept 11; Warwick, UK.
- Hollm-Delgado MG, Allard R, Pilon PA. Invasive group A streptococcal infections, clinical manifestations and their predictors, Montreal, 1995–2001. Emerg Infect Dis. 2005;11:77–82.PubMedGoogle Scholar
- O’Brien KL, Beall B, Barrett NL, Cieslak PR, Reingold A, Farley MM, Epidemiology of invasive group A streptococcus disease in the United States, 1995–1999. Clin Infect Dis. 2002;35:268–76. DOIPubMedGoogle Scholar
- Nelson RJ, Drazen DL. Melatonin mediates seasonal changes in immune function. Ann N Y Acad Sci. 2000;917:404–15.PubMedGoogle Scholar
- Cannell JJ, Vieth R, Umhau JC, Holick MF, Grant WB, Madronich S, Epidemic influenza and vitamin D. Epidemiol Infect. 2006;134:1129–40. DOIPubMedGoogle Scholar
- Brisson J, Bérubé S, Diorio C, Sinotte M, Pollak M, Mâsse B. Synchronized seasonal variations of mammographic breast density and plasma 25-hydroxyvitamin D. Cancer Epidemiol Biomarkers Prev. 2007;16:929–33. DOIPubMedGoogle Scholar
- Lim HS, Roychoudhuri R, Peto J, Schwartz G, Baade P, Moller H. Cancer survival is dependent on season of diagnosis and sunlight exposure. Int J Cancer. 2006;119:1530–6. DOIPubMedGoogle Scholar
- McNeil SA, Halperin SA, Langley JM, Smith B, Warren A, Sharratt GP, Safety and immunogenicity of 26-valent group A streptococcus vaccine in healthy adult volunteers. Clin Infect Dis. 2005;41:1114–22. DOIPubMedGoogle Scholar
Figures
Table
Cite This ArticleTable of Contents – Volume 15, Number 8—August 2009
| EID Search Options |
|---|
|
|
|
|
|
|


Please use the form below to submit correspondence to the authors or contact them at the following address:
Theresa L Lamagni, HCAI and AMR Department, Health Protection Agency, Centre for Infections, 61 Colindale Ave, London NW9 5EQ, UK
Top