Volume 23, Number 2—February 2017
Dispatch
Biofilm-Forming Capability of Highly Virulent, Multidrug-Resistant Candida auris
Abstract
The emerging multidrug-resistant yeast pathogen Candida auris has attracted considerable attention as a source of healthcare–associated infections. We report that this highly virulent yeast has the capacity to form antifungal resistant biofilms sensitive to the disinfectant chlorhexidine in vitro.
The yeast pathogen Candida auris was first detected in 2009 from an ear canal infection in Japan (1). This species initially attracted attention because of its reduced susceptibility to azoles and amphotericin B, combined with the lack of reliable culture-based methods for its identification (2). More recently, C. auris has been associated globally with life-threatening invasive diseases, such as bloodstream and wound infections. C. auris has also caused hospital outbreaks across Asia and South America, as highlighted in a 2016 clinical alert (3). In addition, in a UK intensive care unit, candidemia developed in 20% of patients colonized with C. auris (4). Although the mode of transmission within hospitals is unknown, C. auris may substantially contaminate rooms of colonized or infected patients (5). Phospholipase and proteinase activity have been identified as virulence factors (6); however, because previously used assessment techniques were rudimentary, this pathogen’s ability to form biofilm remains under question (7). The draft genome identifying various proteins involved in biofilm formation (8), coupled with recent descriptions of aggregative and nonaggregative phenotypes, the latter of which are more virulent in vivo (9), indicate the possibility of heterogeneous C. auris biofilm formation, as described for C. albicans (10). We sought to examine these aggregative and nonaggregative C. auris phenotypes in the context of biofilm-forming capacity, investigate their susceptibility to a panel of antifungal agents and the skin disinfectant chlorhexidine, and investigate their virulence in vivo.
Throughout this study, we used C. albicans SC5314 and Candida glabrata WT2001 as comparators for C. auris nonaggregative strains NCPF 8971 (strain 10) and NCPF 8973 (strain 12) and aggregative strains NCPF 8977 (strain 2) and NCPF 8978 (strain 6), as previously described (9). Strains were propagated in YPD broth (Sigma-Aldrich, Dorset, UK), incubated overnight at 30°C, and adjusted to 106 cells/mL in RPMI 1640 medium (11). On 3 separate occasions, 8 biofilms of each Candida species were grown in flat-bottomed, 96-well polystyrene microtiter plates and incubated for 24 h at 37°C, after which biomass was assessed by crystal violet assay (12). C. albicans displayed the greatest biofilm mass (Figure 1, panel A), consistent with previous findings (10). Compared with C. albicans, all C. auris strains formed significantly reduced biofilms (p<0.0001): biomass for nonaggregative C. auris strains 10 and 12 was 2.4 and 1.5 times less, respectively, than those for C. albicans, and biomass for aggregative C. auris strains 2 and 6 was 3.0 and 3.1 times less, respectively. However, these strains formed significantly greater biofilms (p<0.0001) than those formed by C. glabrata (3.8, 6.0, 3.0, and 2.9 times more for strains 10, 12, 2, and 6, respectively). We confirmed these findings for each species by scanning electron microscopy after growing the strains on Thermanox Coverslips (Thermo Fisher Scientific, Paisley, UK) for 24 h, as previously described (12). C. albicans biofilms were typically densely packed with hyphae (Figure 1, panel B), whereas C. glabrata formed a sparse biofilm consisting of yeast cells only, without extracellular matrix (Figure 1, panel C). C. auris strain 10 biofilm formation was intermediate to the C. albicans and C. glabrata phenotypes, showing predominately budding yeast and occasional pseudohyphae (Figure 1, panel D). In agreement with previous findings (9), all tested C. auris strains displayed the same phenotype.
To determine MICs for planktonic and sessile cells of the C. auris strains, we performed antifungal susceptibility testing using standardized Clinical Laboratory Standards Institute M27-A3 broth microdilution (visual inspection) and standardized candidal biofilm testing (metabolic viability) with fluconazole, voriconazole, caspofungin, micafungin, liposomal amphotericin B, amphotericin B, and chlorhexidine (13,14). Antifungal agents were tested in serial 2-fold dilutions (0.06–32.0 mg/L) for planktonic and sessile cells. Fluconazole was ineffective (MICs of >32 mg/L) against planktonic and sessile communities, whereas voriconazole displayed minimal activity against planktonic cells (Table 1, 2). Although liposomal amphotericin B was active against planktonic C. auris at 0.25–1.0 mg/L, up to 16 mg/L was required to reduce biofilm metabolic viability by 90%. Amphotericin B was more effective, requiring 4 mg/L to kill biofilms. Micafungin was the most active echinocandin, requiring <0.5 mg/L to inhibit planktonic cells, compared with 2–32 mg/L for caspofungin. However, these 2 antifungal agents were ineffective against biofilms, requiring >32 mg/L to inhibit sessile cells. Of note, chlorhexidine exhibited the greatest activity, requiring <0.02% to effectively inhibit planktonic and sessile cells across all strains tested. All strains showed similar sensitivity profiles, with the exception of strain 10, for which voriconazole was required in higher concentrations and caspofungin in lower concentrations to effectively inhibit planktonic growth.
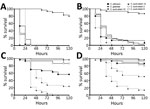
Killing assays in Galleria mellonella were performed, as previously described (12), to assess the pathogenicity of each Candida species. Ten G. mellonella larvae (Livefoods Direct Ltd, Sheffield, UK) with bodyweights of ≈300 mg were used for each test group. Standardized inoculums of 106 and 105 and to 5 × 105 and 5 × 104 cells/larvae (Figure 2) in PBS, were injected into the hemocoel, as previously described (9). We assessed pathogenicity using a Kaplan-Meier plot, monitoring the percent survival over 5 days. Survival data for 5 × 105 cells/larvae showed a significant difference in the killing of larvae by C. glabrata and the other Candida species (p<0.0001) (Figure 2, panel B). Although C. albicans and C. auris had similar kill kinetics in this model, infection with nonaggregative C. auris strain 10 achieved a 100% death rate within 48 h, compared with a rate of ≈87% with C. albicans (p = 0.3076). Moreover, nonaggregative C. auris was significantly more pathogenic than C. albicans when a lower inoculum of 105 (p<0.05) and 5 × 104 cells/larvae (p<0.01) was administered. These data, along with those of Borman et al. (9), suggest that the nonaggregative C. auris phenotype has the capacity to form biofilms with enhanced virulence capacity.
Biofilm formation is a key driver of C. albicans pathogenicity and is associated with patient death (10,15). We show that C. auris can differentially adhere to polymeric surfaces, form biofilms, and resist antifungal agents that are active against its planktonic counterparts. Of particular interest, caspofungin was predominately inactive against C. auris biofilms; this finding was unexpected because caspofungin is normally highly effective against Candida biofilms. These features contribute not only to C. auris virulence but also to its survival in hospital environments, increasing its ability to cause outbreaks (5). The results of the in vivo model used in this study are in line with our clinical experience and validated by findings in other in vivo studies (9), affirming that C. auris is highly virulent or more virulent than C. albicans.
Although unable to form biofilms equivalent to C. albicans, C. auris has a noteworthy virulence capacity that merits further exploration, particularly given the apparent heterogeneity associated with aggregative capacity. These factors, together with the innate resistance of C. auris to most antifungal agents, may explain why it is an emerging pathogen. Our findings suggest it is improbable that the spread and prevalence of C. auris can be controlled with antifungal stewardship approaches alone. We showed that chlorhexidine is effective against C. auris planktonic and sessile communities. Thus, use of this disinfectant can be advocated for topical control of C. auris at standard concentrations used for skin and wound cleansing and disinfection (0.05%–4.0%). Infection-prevention measures targeting C. auris biofilms in patients, on medical devices (e.g., equipment in contact with patients), and in the hospital environment will be required.
Dr. Sherry works as a medical mycologist at the University of Glasgow, Glasgow, UK. Her specific interest is fungal biofilms of clinical significance.
References
- Satoh K, Makimura K, Hasumi Y, Nishiyama Y, Uchida K, Yamaguchi H. Candida auris sp. nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol Immunol. 2009;53:41–4. DOIPubMedGoogle Scholar
- Kathuria S, Singh PK, Sharma C, Prakash A, Masih A, Kumar A, et al. Multidrug-resistant Candida auris misidentified as Candida haemulonii: characterization by matrix-assisted laser desorption ionization-time of flight mass spectrometry and DNA sequencing and its antifungal susceptibility profile variability by Vitek 2, CLSI broth microdilution, and Etest method. J Clin Microbiol. 2015;53:1823–30. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Clinical alert to US healthcare facilities—June 2016. Global emergence of invasive infections caused by the multidrug-resistant yeast Candida auris. 2016 [cited 2016 Jun 24]. http://www.cdc.gov/fungal/diseases/candidiasis/candida-auris-alert.html
- Public Health England. Candida auris identified in England. 2016 [cited 2016 Jul 1]. https://www.gov.uk/government/publications/candida-auris-emergence-in-england/candida-auris-identified-in-england
- Calvo B, Melo AS, Perozo-Mena A, Hernandez M, Francisco EC, Hagen F, et al. First report of Candida auris in America: Clinical and microbiological aspects of 18 episodes of candidemia. J Infect. 2016;73:369–74. DOIPubMedGoogle Scholar
- Kumar D, Banerjee T, Pratap CB, Tilak R. Itraconazole-resistant Candida auris with phospholipase, proteinase and hemolysin activity from a case of vulvovaginitis. J Infect Dev Ctries. 2015;9:435–7. DOIPubMedGoogle Scholar
- Oh BJ, Shin JH, Kim MN, Sung H, Lee K, Joo MY, et al. Biofilm formation and genotyping of Candida haemulonii, Candida pseudohaemulonii, and a proposed new species (Candida auris) isolates from Korea. Med Mycol. 2011;49:98–102. DOIPubMedGoogle Scholar
- Chatterjee S, Alampalli SV, Nageshan RK, Chettiar ST, Joshi S, Tatu US. Draft genome of a commonly misdiagnosed multidrug resistant pathogen Candida auris. BMC Genomics. 2015;16:686. DOIPubMedGoogle Scholar
- Borman AM, Szekely A, Johnson EM. Comparative pathogenicity of United Kingdom isolates of the emerging pathogen Candida auris and other key pathogenic Candida species. mSphere. 2016;1:pii:e00189-16.
- Rajendran R, Sherry L, Nile CJ, Sherriff A, Johnson EM, Hanson MF, et al. Biofilm formation is a risk factor for mortality in patients with Candida albicans bloodstream infection-Scotland, 2012-2013. Clin Microbiol Infect. 2016;22:87–93. DOIPubMedGoogle Scholar
- Ramage G, Vande Walle K, Wickes BL, López-Ribot JL. Standardized method for in vitro antifungal susceptibility testing of Candida albicans biofilms. Antimicrob Agents Chemother. 2001;45:2475–9. DOIPubMedGoogle Scholar
- Sherry L, Rajendran R, Lappin DF, Borghi E, Perdoni F, Falleni M, et al. Biofilms formed by Candida albicans bloodstream isolates display phenotypic and transcriptional heterogeneity that are associated with resistance and pathogenicity. BMC Microbiol. 2014;14:182. DOIPubMedGoogle Scholar
- Clinical Laboratory Standards Institute (CLSI). Reference method for broth dilution antifungal susceptibility testing of yeasts. Approved standard M27–A3, 3rd ed. Wayne (PA): The Institute; 2008.
- Pierce CG, Uppuluri P, Tristan AR, Wormley FL Jr, Mowat E, Ramage G, et al. A simple and reproducible 96-well plate-based method for the formation of fungal biofilms and its application to antifungal susceptibility testing. Nat Protoc. 2008;3:1494–500. DOIPubMedGoogle Scholar
- Rajendran R, Sherry L, Deshpande A, Johnson EM, Hanson MF, Williams C, et al. A prospective surveillance study of candidaemia: epidemiology, risk factors, antifungal treatment and outcome in hospitalized patients. Front Microbiol. 2016;7:915. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleTable of Contents – Volume 23, Number 2—February 2017
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Riina Rautemaa-Richardson, Education and Research Centre, Wythenshawe Hospital, Southmoor Rd, Manchester M23 9LT, UK
Top