Volume 30, Supplement—October 2024
SUPPLEMENT ISSUE
Articles
Serosurveillance for Plasmodium falciparum Malaria in Peruvian Army Peacekeeping Personnel, Central African Republic, 2021–2022
Abstract
Plasmodium falciparum infection threatens military populations deployed to highly malaria-endemic regions, such as Peruvian Army peacekeepers deployed to Central African Republic. During deployment, malaria cases were identified by microscopy and rapid diagnostic tests. After deployment, we performed malaria diagnosis by malachite green loop-mediated isothermal amplification and photo-induced electron transfer PCR assays. We used ELISA to test for P. falciparum C-terminal 19-kDa region merozoite surface protein 1–specific IgG from 97 peacekeepers. Malaria prevalence during deployment was 33.33% and we detected 4 cases after deployment: P. falciparum (n = 2), P. ovale (n = 1), and Plasmodium spp. (n = 1). IgG surveillance showed a seroprevalence of 31.96% in peacekeepers, who had a high P. falciparum exposure during deployment. Our findings reinforce the necessity of active surveillance in military populations to reduce the risk for introduction of new Plasmodium species and strains into the Americas from malaria-endemic areas.
Malaria is a vectorborne disease that affects persons living or traveling within tropical and subtropical regions around the world. According to the World Health Organization, an estimated 249 million malaria cases occurred in 2022 globally; 93.6% of cases and 95.4% of deaths occurred in Africa (1). Military personnel are at particularly high risk for malaria during deployments. Malaria caused by Plasmodium falciparum can lead to severe symptoms such as fever, chills, headache, and even death, if not identified and treated promptly. Those symptoms can seriously affect the performance of military personnel during the execution of critical operations (2).
A continuous surveillance system using rapid diagnostic tests (RDTs), microscopy, and molecular and serologic diagnostic tools is necessary to determine the absolute risk during deployments to highly malaria-endemic areas. For example, in 2003, a malaria outbreak was reported in 44 US Marines deployed to Liberia who had laboratory-confirmed or suspected P. falciparum infections and required immediate medical evacuation (2). A review concluded that the outbreak was associated with inefficient preventive measures, such as partial adherence to mefloquine and the inadequate use of repellent and bed nets (3). In contrast, military personnel from the United Kingdom successfully deployed to the Democratic Republic of the Congo in the same year and had no reported malaria cases during 512 person-weeks (4). Their success was associated with the use of the ABCD (awareness, bite avoidance, chemoprophylaxis, and diagnosis) program to educate and enforce mission objectives (4). Both scenarios highlight the role of numerous factors, such as preventive measures, the complexity and objectives of the mission, duration of deployment, and respective risk for malaria transmission (5).
The Central African Republic (CAR) also reports high transmission of malaria; ≈2.0 million (36.4%) persons were reported to have suspected or confirmed P. falciparum infections during 2021. United Nations military peacekeeping operations in CAR consist of ≈200 armed forces personnel from Peru who promote and maintain the local security of civilians, support democratic efforts, and provide global humanitarian assistance. Peacekeepers from Peru are at risk for severe clinical manifestations of malaria because they are immunologically naive. Infected peacekeepers could introduce new Plasmodium species or new strains to the Americas upon their return to Peru from deployment. In this study, we evaluated the exposure to P. falciparum malaria infection in military peacekeepers from Peru deployed to CAR during 2021–2022.
Epidemiologic Information and Blood Collection
We collected basic demographic, epidemiologic, and clinical information for malaria case-patients identified in CAR (Figure 1). Whole-blood samples were collected again in Hospital Militar Central Luis Arias Schreiber (the Peruvian Army hospital) in Lima, Peru, 1 month after deployment to evaluate active malaria infection. Upon arrival, military personnel were quarantined for 30 days at an army base in Lima, a nonendemic area for malaria; movement outside the base was completely restricted according to guidelines issued by the Peruvian Army Health Unit. In addition, we randomly selected 97 military peacekeepers (because of limited available testing reagent materials) and collected plasma samples to evaluate exposure to P. falciparum (Figure 1).
Detection of Active Cases
Active Plasmodium infection was detected by Boil and Spin malachite green loop-mediated isothermal amplification (LAMP) assay (6). In brief, every 20-µL reaction contained 2× in-house LAMP buffer 0.2% Tween-20, 1.5 mol Betaine, 2 mmol of dNTP, 0.004% malachite green dye, 320 U/mL of Bst DNA Polymerase (New England Biolabs, https://www.neb.com), and 5 µL of Boil and Spin DNA template from whole blood. We performed an amplification reaction at 63°C for 60 minutes using a mini heat block (BioExpress, https://www.bioexpress.com). Positive samples showed a green color and were confirmed by 2 independent laboratory technician readers.
We performed malaria species determination using photo-induced electron transfer (PET) PCR (7). In brief, the PET genus reaction was performed in a 20 µL volume containing 5 µL of purified DNA from whole blood, 2X TaqMan Environmental Buffer 2.0 (ThermoFisher Scientific, https://www.thermofisher.com), and 250 nmol of genus-forward and FAM-reverse primer. The singleplex PET species-specific reactions contained the same mix but with a concentration of 125 nmol of the HEX-labeled species-specific primer (ThermoFisher Scientific). We used thermal cycling conditions for both genus- and species-specific assays of initial denaturation at 95°C for 10 minutes, 45 cycles of denaturation at 95°C for 10 seconds, and annealing at 60°C for 40 seconds. We used a cycle threshold (Ct) value of <41 to separate positive and negative samples.
ELISA of Human Samples
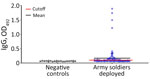
We used plasma samples to screen for IgG seropositivity for P. falciparum C-terminal 19-kDa region merozoite surface protein 1 (MSP1-19) by indirect ELISA as a marker of P. falciparum malaria exposure. We included P. falciparum–negative control plasma samples obtained from 20 persons from Piura Department on the north coast of Peru, a region that has very low malaria incidence. We used those plasma samples to calculate a positivity cutoff value using the average optical density value plus 3 SD on the basis of methods published elsewhere (8).
Statistical Analysis
We performed statistical analysis using Stata version 16.1 statistical software (StataCorp LLC, https://www.stata.com) and Prism software version 9 (GraphPad Software, Inc., https://www.graphpad.com). We used descriptive analysis to demonstrate demographic and epidemiologic characteristics of Peruvian Army peacekeepers and used bivariate analysis to compare characteristics between seropositive and seronegative participants.
Ethics Considerations
Data and sample collections were performed for clinical diagnostic support requested by the Peruvian Army to Naval Medical Research Unit SOUTH. Data and sample analyses were covered by the NAMRU6.2018.0002 protocol (NHSR protocol) approved by Naval Medical Research Unit SOUTH Institutional Review Board. Findings were reported to Peruvian Army authorities for malaria treatment administration, as needed.
Study Population
Out of 205 total peacekeepers deployed to CAR during July 2021–June 2022, only 129 (62.9%) were tested for malaria by microscopy or RDT because they reported malaria-like symptoms. Most (92.2%) participants were men, and a high percentage (57.4%) were warrant officers; mean age was 42.4 (SD 7.4) years. The prevalence of malaria during deployment was 33.3% (43/129) by RDT or microscopy, and the number of malaria episodes experienced ranged from 1 to 4. From that group, 79.1% (34/43) had only 1 episode, 16.3% (7/43) had a second episode, and 1 (2.3%) participant reported having third and fourth episodes of malaria-like symptoms (Table 1). All participants received artemether/lumefantrine and responded adequately to malaria treatment.
In after-deployment samples, LAMP assays detected 4 positive cases out of 129 samples (3.1% positivity), and subsequent molecular method PET-PCR enabled us to further genotype those cases showing 2 P. falciparum, 1 P. ovale, and 1 Plasmodium spp. Of the 4 positive case-patients, 2 (50.0%) reported a malaria episode during their deployment in CAR, and they received the same malaria treatment (artemether/lumefantrine) during deployment as the other positive case-patients.
Regarding malaria exposure, ELISA for MSP1-19–specific IgG demonstrated that 31/97 (31.9%) Peruvian peacekeepers were positive for exposure to P. falciparum malaria (Table 1). Four persons had higher IgG titers than the average positive study population, suggesting a recent malaria infection (Figure 2). Finally, seropositivity was statistically significant between participants in whom malaria was diagnosed in CAR and those in whom it was not (p<0.001) and among persons who were enlisted, warrant officers, and officers (p = 0.026) (Table 2).
Military populations are continuously exposed to P. falciparum during deployments in malaria-endemic regions, resulting in outbreaks, mainly in populations with poor preventive measures. However, disease identification on the basis of symptoms alone could lead to an underestimation of actual transmission and subsequently higher risk for malaria during deployments. In our study, we found that almost one third (31.9%) of peacekeepers deployed to CAR were immunologically exposed to P. falciparum. We also found a significant difference in seropositivity in military personnel in whom malaria was diagnosed in Africa during deployment. The seronegative participants who were malaria-positive in Africa (13.6%; 9/66) could be explained by antibody kinetics, which require weeks after infection to reach significant levels for detection, especially in naive malaria populations. On the other hand, almost half (41.9%; 13/31) of seropositive participants did not receive a malaria diagnosis; this finding could be caused by exposure to Plasmodium parasites that could activate an immune response without a clinical malaria episode. Another possibility could be related to the use of microscopy and RDTs, because these diagnostic methods depend on the skills of laboratory personnel, sample quality, and low parasitemia associated with submicroscopic infections. We do not have information on parasitemia levels to assess the diagnostic capacity of the microscopists and RDTs used during deployment. Diagnosis of active malaria (symptomatic or asymptomatic) should be prioritized using molecular and microscopic tools but could be complemented by serologic analysis in populations with long-term periods of exposure. That finding correlates well with other reports and shows the relevance of serologic surveillance to evaluate exposure to Plasmodium parasites in mobile populations like deployed military personnel (9). This information highlights the need to improve both preventive measures in military personnel and timing of malaria diagnosis (2).
Information is limited about the incidence of malaria in military populations deployed to highly malaria-endemic areas in Africa, especially in social-military conflicted regions. Because of reports of malaria in Somalia and Afghanistan, several military health surveillance systems were implemented (10,11). The US Defense Medical Surveillance System uses a tracking system to determine the area in which malaria was acquired (12). Data from that tracking system are valuable for identifying risk factors related to malaria in military populations, but can be biased by the sample collection process or population type. Identification of military personnel with active malaria infections enables calculation of disease incidence and leads to a better understanding of malaria transmission in this population. However, negative results for malaria on the basis of symptom assessment alone do not necessarily mean that military personnel were not infected during deployment because persons could have been infected without clinical symptoms.
Serologic surveillance in highly malaria-endemic areas offers a tool to determine previous malaria exposure, thereby helping in surveillance efforts to diagnose malaria parasites during symptomatic infection (13). Different antigens can be used for diagnosis, including the liver stage antigen-1 and MSP1-19 (10,11). P. falciparum MSP1 antigens, including MSP1-19, are highly immunogenic during blood-stage Plasmodium and result in sustained IgG titers up to several months after infection (14). Serologic testing can be applied to military populations to determine malaria seroprevalence at the end of deployment, offering complementary information to other diagnostic tools, especially in naive military or civilian populations deployed to highly malaria-endemic regions.
Another relevant finding is the 2 positive non–P. falciparum malaria cases diagnosed after deployment. That result differs from the 2023 World Malaria Report, in which CAR reported >2 million malaria cases, 100% of which were P. falciparum (1). Non–P. falciparum malaria has different biologic and clinical manifestations than P. falciparum malaria. Accurate Plasmodium species diagnosis is key to reducing complications, including relapse because of inadequate malaria treatment for hypnozoites in P. vivax or P. ovale cases. The 2 cases we detected were not the first reported P. ovale cases in military personnel returning to Peru from CAR, highlighting the need for better postdeployment evaluation of personnel to prevent introduction of new Plasmodium species (15). The possibility of contracting non–P. falciparum malaria from other countries in Africa is low because returning personnel were quarantined in Lima, a non–malaria-endemic area, for 30 days after deployment.
The first limitation of our study is that we did not have a predeployment sample to evaluate serologic performance against P. falciparum MSP1-19; only self-reports of no previous travel to malaria-endemic regions were available. Second, malaria diagnosis was performed only in symptomatic persons during deployment, and some subjects could have had asymptomatic malaria. Finally, data about compliance to preventive measures (malaria prophylaxis, use of mosquito repellent or bed nets) or other factors that could modify the risk for malaria were unavailable. Those limitations should be considered in future studies in deployed military personnel to highly malaria-endemic areas.
Our results showed that one third of Peruvian Army military peacekeepers deployed to CAR during 2021–2022 were exposed to P. falciparum. Although few sporadic malaria cases were reported in personnel returning from the African region (15), those findings reinforce the need for additional tools to measure malaria exposure and to implement preventive measures to reduce malaria risk, thereby decreasing infections in civilian and military populations deployed to highly malaria-endemic areas.
Mr. Ventocilla is a Vysnova employee contracted to the Parasitology Department at US Naval Medical Research Unit SOUTH, Lima, Peru, as a scientist researcher. His research interests focus on the testing and development of novel vaccines and therapies against infectious pathogens, such as malaria and dengue, using invitro and animal models.
Acknowledgments
This work was funded by work unit number P0082_22_N6 from the Global Emerging Infectious Surveillance (GEIS) Program.
The views expressed in this article reflect the results of research conducted by the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, nor the US government.
J.A.V. and J.F.S. conceived, designed, and supervised the project study. J.A.V. performed experiments for evaluation of immunogenicity by ELISA. E.M. and R.S. performed LAMP assays for malaria diagnosis. J.A.V. and J.F.S. performed the data and statistical analyses. M.O. and A.M.D.-F. participated in data and sample collection. J.A.V., J.F.S., H.O.V., and D.L.P. wrote the first draft of the manuscript. J.V.A., J.F.S., H.O.V., E.M., R.S., and D.L.P. wrote the final version of the paper. All authors reviewed, edited, and approved the manuscript.
Some authors are military service members and employees of the US government. This work was prepared as part of their official duties. Title 17, U.S.C., §105 provides that copyright protection under this title is not available for any work of the US government. Title 17, U.S.C., §101 defines a US government work as a work prepared by a military service member or employee of the US government as part of that person’s official duties.
References
- World Health Organization. World malaria report 2023. Geneva: The Organization; 2023.
- Kai L, Ying X, Jie LL, Jinhui W, Quan L. Malaria Among United Nations Peacekeepers in the Democratic Republic of the Congo, South Kivu Area, January 2016-July 2019. Clin Infect Dis. 2020;71:698–700. DOIPubMedGoogle Scholar
- Whitman TJ, Coyne PE, Magill AJ, Blazes DL, Green MD, Milhous WK, et al. An outbreak of Plasmodium falciparum malaria in U.S. Marines deployed to Liberia. Am J Trop Med Hyg. 2010;83:258–65. DOIPubMedGoogle Scholar
- Houston DJ, Tuck JJ. Malaria on a military peacekeeping operation: a case study with no cases. Mil Med. 2005;170:193–5. DOIPubMedGoogle Scholar
- Forshey BM, Morton L, Martin N, Cheng Q, Waters NC, Lee J, et al. Plasmodium falciparum rapid test failures threaten diagnosis and treatment of U.S. military personnel. Mil Med. 2020;185:e1–4.PubMedGoogle Scholar
- Barazorda KA, Salas CJ, Braga G, Ricopa L, Ampuero JS, Siles C, et al. Validation study of Boil & Spin malachite green loop mediated isothermal amplification (B&S MG-LAMP) versus microscopy for malaria detection in the Peruvian Amazon. PLoS One. 2021;16:
e0258722 . DOIPubMedGoogle Scholar - Lucchi NW, Narayanan J, Karell MA, Xayavong M, Kariuki S, DaSilva AJ, et al. Molecular diagnosis of malaria by photo-induced electron transfer fluorogenic primers: PET-PCR. PLoS One. 2013;8:
e56677 . DOIPubMedGoogle Scholar - Ventocilla JA, Tapia LL, Ponce R, Franco A, Leelawong M, Aguiar JC, et al. Evaluation of naturally acquired immune responses against novel pre-erythrocytic Plasmodium vivax proteins in a low endemic malaria population located in the Peruvian Amazon Basin. Malar J. 2024;23:163. DOIPubMedGoogle Scholar
- Kartal L, Mueller I, Longley RJ. Using serological markers for the surveillance of Plasmodium vivax malaria: a scoping review. Pathogens. 2023;12:791. DOIPubMedGoogle Scholar
- Plucinski MM, Candrinho B, Chambe G, Muchanga J, Muguande O, Matsinhe G, et al. Multiplex serology for impact evaluation of bed net distribution on burden of lymphatic filariasis and four species of human malaria in northern Mozambique. PLoS Negl Trop Dis. 2018;12:
e0006278 . DOIPubMedGoogle Scholar - Rogier E, Wiegand R, Moss D, Priest J, Angov E, Dutta S, et al. Multiple comparisons analysis of serological data from an area of low Plasmodium falciparum transmission. Malar J. 2015;14:436. DOIPubMedGoogle Scholar
- Military Health System. Update: malaria, U.S. Armed Forces, 2021–2022 [cited 2024 Feb 23]. https://health.mil/News/Articles/2022/03/01/Update-Mal-MSMR
- Tayipto Y, Liu Z, Mueller I, Longley RJ. Serology for Plasmodium vivax surveillance: A novel approach to accelerate towards elimination. Parasitol Int. 2022;87:
102492 . DOIPubMedGoogle Scholar - Mueller I, Galinski MR, Tsuboi T, Arevalo-Herrera M, Collins WE, King CL. Natural acquisition of immunity to Plasmodium vivax: epidemiological observations and potential targets. Adv Parasitol. 2013;81:77–131. DOIPubMedGoogle Scholar
- Guerra RI, Ore M, Valdivia HO, Bishop DK, Ramos M, Mores CN, et al. A cluster of the first reported Plasmodium ovale spp. infections in Peru occuring among returning UN peace-keepers, a review of epidemiology, prevention and diagnostic challenges in nonendemic regions. Malar J. 2019;18:176. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: November 11, 2024
Table of Contents – Volume 30, Supplement—October 2024
| EID Search Options |
|---|
|
|
|
|
|
|

Please use the form below to submit correspondence to the authors or contact them at the following address:
Juan F. Sanchez, Naval Medical Research Unit SOUTH, Avenida Venezuela Cdra. 36 s/n, Bellavista, Callao, Peru
Top