Volume 30, Number 1—January 2024
Research
Population-Based Study of Pertussis Incidence and Risk Factors among Persons >50 Years of Age, Australia
Abstract
Despite vaccination programs, pertussis has been poorly controlled, especially among older adults in Australia. This longitudinal, retrospective, observational study aimed to estimate the incidence and risk factors of pertussis among persons ≥50 years of age in Australia in the primary care setting, including those with underlying chronic obstructive pulmonary disease (COPD) or asthma. We used the IQVIA general practitioner electronic medical record database to identify patients ≥50 years of age with a clinical diagnosis of pertussis during 2015–2019. Pertussis incidence rates ranged from 57.6 to 91.4 per 100,000 persons and were higher among women and highest in those 50–64 years of age. Patients with COPD or asthma had higher incidence rates and an increased risk for pertussis compared with the overall population ≥50 years of age. Our findings suggest that persons ≥50 years of age in Australia with COPD or asthma have a higher incidence of and risk for pertussis diagnosis.
Pertussis, or whooping cough, a bacterial respiratory infection caused by Bordetella pertussis, is typically characterized by paroxysms of coughing with a whooping sound during inhalation. In Australia, pertussis is one of the least well-controlled vaccine-preventable diseases (1). Robust childhood and maternal immunization programs prevent pertussis-related hospitalizations and mortality in infants and children, but breakthrough disease can occur at any age, because naturally acquired and vaccine-induced immunity against pertussis is not lifelong (2,3). Although older adults can be a source of transmission and adversely affected by infection, vaccination programs are prioritized for pregnant women (preferably 20–32 weeks’ gestation), infants and children (i.e., ages 2, 4, 6 and 18 months, and 4 years), and adolescents (11–13 years of age) (1). Consequently, pertussis in older adults constitutes a considerable reservoir of infection and contributes to substantial disease burden, healthcare utilization, and other pertussis-associated costs (1).
Recent research has offered a clearer assessment of pertussis cases among adults ≥50 years of age (4). In Australia, pertussis-containing (i.e., combined diphtheria, tetanus, and acellular pertussis) vaccines are recommended for adults at 50 years and 65 years of age by the Australian Technical Advisory Group on Immunisation (1,5,6) but are not funded by the National Immunisation Program. Both confirmed and probable cases of pertussis must be reported to the Commonwealth’s National Notifiable Diseases Surveillance System (NNDSS) (5). However, pertussis infections are often underdiagnosed and underreported, owing to difficulties in diagnosis because of unspecific symptoms, delays in seeking healthcare, underuse of diagnostic testing by general practitioners (GPs), and other coexisting respiratory diseases. Accordingly, NNDSS notification data tend to underestimate the true number of pertussis infections and are more likely to capture persons with severe disease (7), posing serious challenges to policy considerations for pertussis vaccination in adults ≥50 years of age. Given the underuse of diagnostic testing by GPs, pertussis diagnoses are based frequently on clinical evidence. Beyond NNDSS data, alternative sources of data, including electronic medical records (EMRs), may inform understanding of the burden of pertussis in persons ≥50 years of age in Australia (hereafter Australians >50 years) in the primary care setting.
Patients with underlying respiratory conditions, such as asthma and chronic obstructive pulmonary disease (COPD), have an increased risk for pertussis, leading to more severe outcomes and exacerbation of asthma and COPD (8–10). The considerable overlap in the clinical manifestations of those conditions can complicate the diagnosis of pertussis in such patients. In this study, we estimated the incidence rate (IR) of pertussis based on clinical diagnoses and determined the risk factors of pertussis among Australians ≥50 years, including those with COPD or asthma, using the IQVIA GP EMR database.
Data Sources
We conducted a longitudinal, retrospective, observational study by using records in the IQVIA GP EMR database dated January 2015–December 2019. The IQVIA GP EMR database contains de-identified patient records collected from the EMR software of consenting GPs in Australia, covering 2,286,308 patients across 2,500 GPs and averaging 6 years’ follow-up per patient. The database provides rich data that includes demographic and biometric profiles, medical profiles, prescribing information, and prescriber characteristics.
Study Population
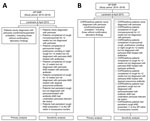
The study population included patients ≥50 years of age whose records were collected in the IQVIA GP EMR database during January 2015–December 2019, with pertussis as the outcome of interest. We identified pertussis cases in the overall study population and in patients with COPD or asthma (Figure 1). We used search terms to identify pertussis, COPD, and asthma cases for the primary and sensitivity analyses (Appendix Table 1). We performed sensitivity analyses on a secondary patient population, applying a broader pertussis definition to assess the robustness of estimates, including patients with prolonged coughing potentially related to undiagnosed pertussis, treated empirically as atypical pneumonia or upper respiratory tract infections (Appendix Table 2).
We excluded patients with a diagnosis of pertussis before April 30, 2015, because a run-in period was required to rule out prevalent cases carried forward from the end of 2014. We also excluded patients without a history of diagnosed pertussis during the study period who visited their GP for pertussis vaccination or travel immunization.
Study Objectives
The primary objective of our study was to estimate pertussis incidence based on clinical evidence captured in the IQVIA GP EMR database in Australians ≥50 years, including those with COPD or asthma. The secondary objective was to determine the risk factors for pertussis in this population.
Data Analysis
We calculated the IR of pertussis (cases/100,000 persons) in the overall study population and in patients with COPD or asthma per calendar year as the number of new cases of pertussis divided by the corresponding population in the dataset for each year. We parametrically estimated IRs with 95% CIs by fitting Poisson or negative binomial distributions as appropriate. We compared qualitative or discrete variables by using Pearson χ2 or Fisher exact tests, and we compared quantitative variables by using 2-sample Student t-test or analysis of variance, after checking equality of variance (Fisher test) and normality (Shapiro–Wilk test). We used Wilcoxon, Mann–Whitney, or Kruskal–Wallis tests if equality of variance and normality were not confirmed.
To determine risk factors for pertussis, we compared patients with diagnosed pertussis with controls by using a nested case-control design. We defined controls as patients who had never received a diagnosis of pertussis during the study period. We matched case patients and controls based on age group (in 5-year groups >50 years of age), sex, postal code, and year of GP visit, by using a 1:3 ratio within the same calendar year. We used conditional logistic regression to estimate odds ratios (ORs) and 95% CIs. We examined all exposure variables for univariate associations and constructed a multivariable model that included age, sex, and any variables with p value ≤0.2 in univariate analyses. We also performed multivariable logistic regressions based on forward and backward elimination methods to confirm robustness of the estimates. Given its association with pertussis diagnoses in a previous report, asthma was retained in the final model a priori, irrespective of statistical significance (11). Likewise, use of angiotensin-converting enzyme inhibitors (known to induce cough) or angiotensin receptor blockers (known to protect against pertussis infection) and history of pertussis vaccination (during the study period) were retained in the final model a priori, irrespective of statistical significance (4,12). We performed additional exploratory analyses to evaluate health-seeking behavior by estimating the number of GP visits per year before pertussis diagnosis and antibiotic prescriptions for cough 1 month before pertussis diagnosis; we then further stratified these data by age, sex, and underlying COPD or asthma. We performed all analyses by using R version 4.3 (The R Foundation for Statistical Computing, https://www.r-project.org).
Study Population
The total population of Australians ≥50 years in the IQVIA GP EMR database covered 252,227–415,201 patients for each year during 2015–2019. We selected 992 patients with pertussis, including those not tested for pertussis, for inclusion in the primary analysis based on the diagnosis label (Table 1). Laboratory tests for pertussis were ordered for 243 (24%) patients and results documented for 205 (21%) patients, of which only 10 (0.01%) tested positive for pertussis. Because of the limited diagnostic testing performed for patients with diagnosed pertussis in GP clinics, our study relied instead on the clinical diagnosis of pertussis.
Among 992 patients with diagnosed pertussis, 66% were women, 41% had a history of cardiovascular disease, 19% had COPD, and 12% had asthma; mean age was 63.3 (95% CI 62.7–63.9) years. Fourteen percent of patients had a record of pertussis immunization during the study period and before pertussis diagnosis. A total of 2,543 patients with pertussis met the extended definition of pertussis for the sensitivity analysis (Appendix Tables 3, 4).
Incidence of Pertussis
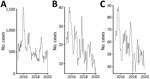
We observed differences in annual incidence of pertussis among Australians ≥50 years in 2015–2019 (Figure 2, panel A; Appendix Table 5). Pertussis IRs per 100,000 persons were 91.4 (95% CI 84.1–98.7) in 2015 and 58.7 (95% CI 51.4–66.0) in 2019 (Figure 2, panel A). In age subgroups, IRs were consistently highest among those 50–64 years of age and 65–74 years of age (Figure 2, panel B; Appendix Table 5). Overall, pertussis IRs varied across all age groups during 2015–2019 (Figure 2, panel B).
When stratified by sex, pertussis IRs among women were 110.5 (95% CI 102.3–118.7) in 2015 and 74.5 (95% CI 66.3–82.7) in 2019. Lower IRs of 70.6 (95% CI 64.3–76.8) in 2015 and 41.6 (95% CI 35.4–47.8) in 2019 were observed among men (Figure 2, panel C). Similar trends were reported by the NNDSS, although pertussis IRs were lower than those in our study population (Figure 2).
In patients with COPD, pertussis IRs throughout the study period ranged from 304.4 (95% CI 290.7–318.1) in 2015 to 194.3 (95% CI 180.5–207.9) in 2019 (Figure 3, panel A; Appendix Table 6). Similarly, in patients with asthma, pertussis IRs ranged from 473.0 (95% CI 454.0–492.0) in 2015 to 376.8 (95% CI 357.8–395.8) in 2019 (Figure 4, panel A; Appendix Table 7). Although pertussis IRs among patients with COPD or asthma were higher than the overall study population, variations between age groups were generally consistent (Figure 3, panel B; Figure 4, panel B). Consistent with the overall study population, pertussis IRs in women with COPD or asthma were higher than in men with COPD (Figure 3, panel C; Appendix Table 6) or in men with asthma (Figure 4, panel C; Appendix Table 7).
In the sensitivity analysis, based on an extended definition of pertussis, annual IRs were 197.6 (95% CI 185.5–209.7) in 2015 and 196.7 (95% CI 184.5–208.8) in 2019 (Appendix Figure 1, panel A). Overall, the lowest IRs were observed in patients ≥85 years of age (Appendix Figure 1, panel B). IRs remained higher among women versus men (Appendix Figure 1, panel C). In the sensitivity analysis, IRs among patients with COPD or asthma were higher than those in the overall study population (Appendix Figure 2, panel A, Figure 3, panel A). In 2016–2018, pertussis IRs in patients with COPD or asthma were highest in patients 65–74 years of age (Appendix Figure 2, panel B, Figure 3, panel B). Overall, IRs by age group and sex in patients with COPD or asthma were higher than IRs for the same group in the primary analysis and NNDSS, consistent with trends observed in the primary analysis (Appendix Figure 2, panels B, C, Figure 3, panels B, C). Trends observed in the monthly number of pertussis cases defined within the primary and sensitivity analyses cohorts and those reported in the NNDSS data were generally consistent and peaked in winter (June–September) (Figure 5).
Risk Factor Modeling
Conditional univariable logistic regression models predicted that concurrent diabetes, asthma, or COPD, use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, and prior use of antibiotics within 1 month increased the risk for a pertussis diagnosis; history of influenza vaccination was associated with reduced risk for a pertussis diagnosis (Table 2). The adjusted multivariable logistic regression model suggested that prior prescription of an antibiotic for cough within 1 month (OR 7.00 [95% CI 4.21–11.64]), asthma (OR 2.94 [95% CI 1.71–5.04]), and COPD (OR 1.88 [95% CI 1.23–2.86]) were predictors of pertussis diagnosis, but the risk for pertussis diagnosis was lower for patients with a history of influenza vaccination (OR 0.38 [95% CI 0.26–0.55]; Table 3).
Healthcare-Seeking Behavior and Antibiotic Prescriptions
We compared the number of GP visits for men and women in terms of asthma status, COPD status, and across age groups (Appendix Figure 4, panel A). We observed no sex-specific differences (p = 0.12) among patients with COPD or asthma (women, median 11, interquartile range [IQR] 10, vs. men, median 10, IQR 13).
In the overall study population, the median number of GP visits within 1 year before pertussis diagnosis was significantly higher (p = 0.001) for women (median 8, IQR 10) than for men (median 6, IQR 9). The median number of GP visits increased with presence of COPD or asthma for both women and men. In patients without COPD or asthma, the median number of GP visits was also significantly higher (p = 0.01) in women (median 6, IQR 8) compared with men (median 5, IQR 9). Furthermore, the number of GP visits increased with age, independent of sex and COPD or asthma status (Appendix Figure 4, panels B, C).
To investigate the observed reduced risk for pertussis associated with history of influenza vaccination within the risk factor modeling, we also looked at the distributed number of GP visits among those with or without history of influenza vaccination before pertussis diagnosis. Persons vaccinated for influenza before pertussis diagnosis had a higher median number of GP visits compared with those without influenza vaccination across all age groups (Table 4).
Overall, 252 (25%) patients diagnosed with pertussis in the primary analysis were prescribed antibiotics for cough 1 month before their pertussis diagnosis. The most prescribed antibiotics were macrolides (83%) and broad-spectrum penicillin (24%), followed by tetracyclines (5%), cephalosporins (4%), and trimethoprim combinations (1%) (Table 5).
By using the IQVIA GP EMR database, we estimated IRs and risk factors for clinically diagnosed pertussis among Australians ≥50 years, including those with COPD or asthma (Appendix Figure 5). IRs were highest among patients 50–64 years of age and were 2 times higher in women than in men. Furthermore, compared with the overall study population, IRs in patients with COPD were ≈3–4 times higher and in patients with asthma were ≈5–8 times higher.
In a systematic literature review reporting results from 85 publications, IRs in older adults broadly ranged 2–16,670/100,000 population, depending on the definition of pertussis and study methodology (4). Our findings are largely consistent with previously published global studies and studies in Australia, also reporting higher pertussis IRs in women compared with men (11,13,14). The higher IRs in women may be attributed to healthcare-seeking behavior, increased exposure to children and elderly persons infected with pertussis through caretaker roles, and biological and immune response differences (14).
For the extended definition of pertussis in the sensitivity analysis, we noted pertussis IRs to be higher than those in the primary analysis, likely attributable in part to the inclusion of nonpertussis seasonal respiratory diseases. In patients with COPD or asthma, we found IRs in the sensitivity analysis to be >3 times higher than those observed in the primary analysis, although the overall trends were consistent.
Trends observed in IRs were largely consistent between GP EMR data and NNDSS data, aligning with the known cyclic trend of pertussis epidemics in Australia. Contemporary data suggest that pertussis outbreaks occur periodically every 3 to 4 years (5,15); the 2 most recent epidemics of pertussis in Australia peaked in 2011 and 2015 (16). Evidence of seasonal fluctuations in pertussis incidence has been noted in other countries as well (17–21). There are conflicting findings in the context of Australia; several studies report higher incidence peaks in spring and summer months (November–January) and others report such peaks in winter months (June–September) (22–24). Pertussis was also found to be a common pathogen in infants hospitalized for acute lower respiratory tract infection, including pertussis co-infection, during winter in the Netherlands (25). It is therefore likely that the incidence spikes of pertussis observed in our study were confounded by circulating influenza viruses or respiratory syncytial virus outbreaks because of the the non–laboratory-confirmed definition of pertussis cases.
Conditional multivariable regression analysis showed that prior use of antibiotics within 1 month and concurrent asthma and COPD were predictors of pertussis diagnosis. Because only 24% of patients with pertussis in this study were tested for pertussis, antibiotics prescribed for concurrent asthma and COPD may have influenced prediction of pertussis diagnosis.
Patients with a history of influenza vaccination had a 62% lower risk for pertussis diagnosis than those without that history. A post-hoc analysis from a clinical trial among pregnant women suggested that influenza vaccination may have a positive effect on rates of pertussis infection and called for further investigation into the possible mechanisms in the upper respiratory tract that can lead to the synergy between the 2 pathogens (26). Influenza-vaccinated persons have a lower risk for influenza-related worsening of other respiratory diseases (27); thus, fewer potentially misdiagnosed pertussis cases may contribute to artifacts rather than true association between influenza vaccination history and pertussis diagnosis. Given the low pertussis testing rates in this study, these findings should be treated with caution. Notably, the Australian government offers free influenza vaccines through the National Immunisation Program for seniors ≥65 years of age, which may have contributed to a higher influenza vaccination rate in the study population. In addition, patients in better health or who are health-conscious are more likely to get vaccinated (i.e., healthy vaccinee bias) and seek health care when experiencing respiratory symptoms (28).
The risk for pertussis diagnosis in patients with underlying COPD and asthma was previously reported to be higher than for patients with pertussis but without those conditions (29). Contemporary data also suggest that patients with COPD and asthma have a higher pertussis incidence, risk for pertussis infection, and greater subsequent disease burden than patients with pertussis but without such concurrent conditions (9,29–31). Furthermore, asthma, COPD, and other chronic inflammatory pulmonary diseases can be exacerbated by B. pertussis infection (29). Increased risk for pertussis in patients with COPD or asthma may be explained by potential adverse effects of inhaled or systemic corticosteroids, altered airway architecture, impairment of innate and acquired immunity, waning humoral immunity over time, and influence of concurrent conditions on immunogenicity (30).
In this study, women, older age groups, and those with a history of influenza vaccination were associated with a higher median number of GP visits in a year, likely resulting in a higher chance of pertussis being recognized or diagnosed. Those observations might be due to women and older adults (who may have other concurrent conditions) visiting the GP more often (32–34). The higher median number of GP visits in persons with a history of influenza vaccination versus without suggests that those persons are more health conscious (i.e., healthy vaccinee bias) or had other conditions that required more GP visits. Among all patients diagnosed with pertussis, antibiotic prescriptions within 1 month before pertussis diagnosis were more common for those with COPD or asthma, men, and younger age groups (50–74 years); macrolides and penicillin were the most prescribed. Of note, persistent cough is a criterion for asthma and COPD exacerbation according to Australia guidelines (35,36), possibly explaining why antibiotics were more commonly prescribed and why pertussis may not have been recognized or diagnosed earlier in these patients. Because macrolides are the preferred treatment for pertussis, an adequate dosage and treatment duration may reduce likelihood of pertussis diagnosis (37), which may have skewed the estimated pertussis IRs in the populations described in this study, particularly among patients with COPD or asthma.
Because of differing case definitions in this study and the lack of routine laboratory testing in the primary care setting, the pertussis IRs in Australians ≥50 years may be higher than those reported to the NNDSS. NNDSS data rely on GP clinical, laboratory, or empirical diagnoses to identify confirmed and probable cases of pertussis. The surveillance case definition for pertussis requires confirmed cases to have either laboratory-definitive evidence or laboratory-suggestive evidence and clinical evidence, whereas probable cases require clinical and epidemiologic evidence (38). In our study, we identified cases based on clinical diagnosis, and only a small proportion of patients had pertussis-related diagnostic laboratory tests performed and documented in the EMR. Therefore, the approach we used in this study captured more cases that did not meet the NNDSS case definition of pertussis. Estimating the true impact of pertussis vaccination is not feasible, given the low vaccination rate and underdocumentation of vaccination history in the EMR database. Previous studies have shown that pertussis-related hospitalizations, healthcare burden, concurrent conditions, and risk for death increase with age (4,11,39). However, because the GP EMR database is based in the primary care setting, it is not representative of all Australians ≥50 years and does not allow further evaluation of pertussis severity and its association with hospitalization, healthcare burden, and mortality. Given the known underdiagnosis and underreporting of pertussis, our incidence and risk factor analysis can still provide useful guidance related to pertussis prevention in the primary care setting. Nevertheless, it will be important to further validate the findings of this study by using a more specific and validated case definition of pertussis cases.
From a public health standpoint, this study highlights the importance of pertussis prevention for Australians ≥50 years, especially among those with COPD or asthma, thus improving community awareness and uptake of immunization at age 50 and 65 years, which is currently suboptimal (40,41). An effective vaccination strategy is necessary to reduce complications and increased healthcare costs associated with pertussis among patients with COPD or asthma (4,29). For patients with COPD or asthma who have unrecognized or undiagnosed pertussis, inappropriately prescribed antibiotics may empirically treat pathogens causing other respiratory illnesses but delay the diagnosis and control of pertussis. Conversely, timely pertussis vaccinations can protect vaccinated persons against pertussis development and prevent community-level transmission. Other strategies include increasing pertussis testing by GPs to improve ascertainment of cases and ensure timely treatment (40).
Future studies might consider the effect of policy interventions on pertussis vaccination behavior, underuse of pertussis vaccines, and cost-effectiveness of potential new models of pertussis immunization programs to address policy gaps in the present program. In summary, a sizeable burden of pertussis in older adults in Australia has a greater impact on persons with COPD or asthma. This study highlights the importance of pertussis prevention for Australians ≥50 years of age.
Dr. Pearce is a practicing grass-roots general practitioner and policy adviser in Australia who serves as chairman of the Immunisation Coalition and member of the Asia Pacific Alliance for the Control of Influenza.
Acknowledgments
We thank Roeland Van Kerckhoven for publication management and Co Luu for providing medical insight supporting the interpretation of study results. The authors also thank Costello Medical for editorial assistance and publication coordination, on behalf of GSK, and acknowledge Loveena Sharma for medical writing and editorial assistance based on the authors’ input and direction.
The data and datasets that support the findings of this study are not publicly available because they are owned by IQVIA.
This study was sponsored by GlaxoSmithKline Biologicals SA (Study identifier eTrack: EPI-pertussis-066). Support for third-party writing assistance for this article, provided by Loveena Sharma, Costello Medical, Singapore, and Claire Hews, Costello Medical, UK, was funded by GSK in accordance with Good Publication Practice (GPP3) guidelines (https://www.ismpp.org/gpp3).
R.P. has received honoraria from GSK group of companies and Pfizer for educational speaking events and advisory board participation. J.C., A.G., and S.S. are employees of and hold shares in the GSK group of companies. L.-A.L. is an employee of the GSK group of companies. K.L.C., B.S., and G.S. are employees of IQVIA and received fees related to the conduct of this study from the GSK group of companies. C.R.M. reports nothing to disclose.
Substantial contributions to study conception and design: R.P., J.C., K.L.C., A.G., L.-A.L., C.R.M., B.S., G.S., and S.S.; substantial contributions to analysis and interpretation of the data: R.P., J.C., K.L.C., A.G., L.-A.L., B.S., G.S., and S.S.; drafting the article or revising it critically for important intellectual content: R.P., J.C., K.L.C., A.G., L.-A.L., C.R.M., B.S., G.S., and S.S.; final approval of the version of the article to be published: R.P., J.C., K.L.C., A.G., L.-A.L., C.R.M., B.S., G.S., and S.S.
References
- Australian Government Department of Health. Pertussis (whooping cough) 2021 [cited 2023 Jul 13]. https://immunisationhandbook.health.gov.au/vaccine-preventable-diseases/pertussis-whooping-cough
- Burdin N, Handy LK, Plotkin SA. What is wrong with pertussis vaccine immunity? The problem of waning effectiveness of pertussis vaccines. Cold Spring Harb Perspect Biol. 2017;9:
a029454 . DOIPubMedGoogle Scholar - Crowcroft NS, Pebody RG. Recent developments in pertussis. Lancet. 2006;367:1926–36. DOIPubMedGoogle Scholar
- Kandeil W, Atanasov P, Avramioti D, Fu J, Demarteau N, Li X. The burden of pertussis in older adults: what is the role of vaccination? A systematic literature review. Expert Rev Vaccines. 2019;18:439–55. DOIPubMedGoogle Scholar
- Australian Technical Advisory Group on Immunisation (ATAGI). Pertussis. In: The Australian immunisation handbook, 10th edition. Canberra: Australian Government Department of Health; 2015. p. 312–26.
- Australian Government Department of Health and Aged Care. Australian Technical Advisory Group on Immunisation (ATAGI) 2023 [cited 2023 Jul 13]. https://www.health.gov.au/committees-and-groups/australian-technical-advisory-group-on-immunisation-atagi
- Karki S, McIntyre P, Newall AT, MacIntyre CR, Banks E, Liu B. Risk factors for pertussis hospitalizations in Australians aged 45 years and over: A population based nested case-control study. Vaccine. 2015;33:5647–53. DOIPubMedGoogle Scholar
- Hashemi SH, Nadi E, Hajilooi M, Seif-Rabiei MA, Samaei A. High seroprevalence of Bordetella pertussis in patients with chronic obstructive pulmonary disease: a case-control study. Tanaffos. 2015;14:172–6.PubMedGoogle Scholar
- Bhavsar A, Aris E, Harrington L, Simeone JC, Ramond A, Lambrelli D, et al. Burden of pertussis in individuals with a diagnosis of asthma: a retrospective database study in England. J Asthma Allergy. 2022;15:35–51. DOIPubMedGoogle Scholar
- Jenkins VA, Savic M, Kandeil W. Pertussis in high-risk groups: an overview of the past quarter-century. Hum Vaccin Immunother. 2020;16:2609–17. DOIPubMedGoogle Scholar
- Liu BC, McIntyre P, Kaldor JM, Quinn HE, Ridda I, Banks E. Pertussis in older adults: prospective study of risk factors and morbidity. Clin Infect Dis. 2012;55:1450–6. DOIPubMedGoogle Scholar
- Dicpinigaitis PV. Angiotensin-converting enzyme inhibitor-induced cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(Suppl):169S–73S. DOIPubMedGoogle Scholar
- Leong RNF, Wood JG, Liu B, Menzies R, Newall AT. Estimating pertussis incidence in general practice using a large Australian primary care database. Vaccine. 2021;39:4153–9. DOIPubMedGoogle Scholar
- Peer V, Schwartz N, Green MS. A multi-country, multi-year, meta-analytic evaluation of the sex differences in age-specific pertussis incidence rates. PLoS One. 2020;15:
e0231570 . DOIPubMedGoogle Scholar - Quinn HE, McIntyre PB. Pertussis epidemiology in Australia over the decade 1995-2005—trends by region and age group. Commun Dis Intell Q Rep. 2007;31:205–15.PubMedGoogle Scholar
- NNDSS Annual Report Working Group. Australia’s notifiable disease status, 2016: annual report of the National Notifiable Diseases Surveillance System. Canberra: Australian Government Department of Health; 2021 [cited 2022 Oct 19]. https://www1.health.gov.au/internet/main/publishing.nsf/Content/5C71FABF639650F6CA2586520081286B/$File/australia_s_notifiable_disease_status_2016_annual_report_of_the_national_notifiable_diseases_surveillance_system.pdf
- Gu W, Wang K, Zhang X, Hao C, Lu Y, Wu M, et al. Pathogen analysis of pertussis-like syndrome in children. BMC Infect Dis. 2020;20:353. DOIPubMedGoogle Scholar
- Skowronski DM, De Serres G, MacDonald D, Wu W, Shaw C, Macnabb J, et al. The changing age and seasonal profile of pertussis in Canada. J Infect Dis. 2002;185:1448–53. DOIPubMedGoogle Scholar
- Ghorbani GR, Zahraei SM, Moosazadeh M, Afshari M, Doosti F. Comparing seasonal pattern of laboratory confirmed cases of pertussis with clinically suspected cases. Osong Public Health Res Perspect. 2016;7:131–7. DOIPubMedGoogle Scholar
- Bhatti MM, Rucinski SL, Schwab JJ, Cole NC, Gebrehiwot SA, Patel R. Eight-year review of Bordetella pertussis testing reveals seasonal pattern in the United States. J Pediatric Infect Dis Soc. 2017;6:91–3. DOIPubMedGoogle Scholar
- Public Health England. Laboratory confirmed cases of pertussis in England: annual report for 2019. London: Public Health England; 2020 [cited 2022 Aug 15]. https://assets.publishing.service.gov.uk/media/5ea6bcf5e90e07048c84e801/hpr0820_PRTSSS_annual.pdf
- Leong RNF, Wood JG, Turner RM, Newall AT. Estimating seasonal variation in Australian pertussis notifications from 1991 to 2016: evidence of spring to summer peaks. Epidemiol Infect. 2019;147:
e155 . DOIPubMedGoogle Scholar - Kaczmarek MC, Ware RS, Nimmo GR, Robson JMB, Lambert SB. Pertussis seasonality evident in polymerase chain reaction and serological testing data, Queensland, Australia. J Pediatric Infect Dis Soc. 2016;5:214–7. DOIPubMedGoogle Scholar
- Huang X, Lambert S, Lau C, Soares Magalhaes RJ, Marquess J, Rajmokan M, et al. Assessing the social and environmental determinants of pertussis epidemics in Queensland, Australia: a Bayesian spatio-temporal analysis. Epidemiol Infect. 2017;145:1221–30. DOIPubMedGoogle Scholar
- van den Brink G, Wishaupt JO, Douma JC, Hartwig NG, Versteegh FGA. Bordetella pertussis: an underreported pathogen in pediatric respiratory infections, a prospective cohort study. BMC Infect Dis. 2014;14:526. DOIPubMedGoogle Scholar
- Nunes MC, Cutland CL, Madhi SA. Influenza vaccination during pregnancy and protection against pertussis. N Engl J Med. 2018;378:1257–8. DOIPubMedGoogle Scholar
- Centers for Disease Control and Prevention. Vaccine effectiveness: how well do flu faccines work? 2022 [cited 2022 Dec 13]. https://www.cdc.gov/flu/vaccines-work/vaccineeffect.htm
- Remschmidt C, Wichmann O, Harder T. Frequency and impact of confounding by indication and healthy vaccinee bias in observational studies assessing influenza vaccine effectiveness: a systematic review. BMC Infect Dis. 2015;15:429. DOIPubMedGoogle Scholar
- Buck PO, Meyers JL, Gordon L-D, Parikh R, Kurosky SK, Davis KL. Economic burden of diagnosed pertussis among individuals with asthma or chronic obstructive pulmonary disease in the USA: an analysis of administrative claims. Epidemiol Infect. 2017;145:2109–21. DOIPubMedGoogle Scholar
- Capili CR, Hettinger A, Rigelman-Hedberg N, Fink L, Boyce T, Lahr B, et al. Increased risk of pertussis in patients with asthma. J Allergy Clin Immunol. 2012;129:957–63. DOIPubMedGoogle Scholar
- Aris E, Harrington L, Bhavsar A, Simeone JC, Ramond A, Papi A, et al. Burden of pertussis in COPD: a retrospective database study in England. COPD. 2021;18:157–69. DOIPubMedGoogle Scholar
- Thompson AE, Anisimowicz Y, Miedema B, Hogg W, Wodchis WP, Aubrey-Bassler K. The influence of gender and other patient characteristics on health care-seeking behaviour: a QUALICOPC study. BMC Fam Pract. 2016;17:38. DOIPubMedGoogle Scholar
- Wang Y, Hunt K, Nazareth I, Freemantle N, Petersen I. Do men consult less than women? An analysis of routinely collected UK general practice data. BMJ Open. 2013;3:
e003320 . DOIPubMedGoogle Scholar - Xu KT, Borders TF. Gender, health, and physician visits among adults in the United States. Am J Public Health. 2003;93:1076–9. DOIPubMedGoogle Scholar
- COPD-X. Manage eXacerbations. The COPD-X Plan: Australian and New Zealand guidelines for the management of chronic obstructive pulmonary disease. 2021 [cited 2022 Aug 15]. https://copdx.org.au/copd-x-plan/x-manage-exacerbations
- National Asthma Council Australia. Managing flare-ups in adults. Australian Asthma Handbook. 2022 [cited 2023 Jul 13]. https://www.asthmahandbook.org.au/management/adults/flare-ups
- Bergquist SO, Bernander S, Dahnsjö H, Sundelöf B. Erythromycin in the treatment of pertussis: a study of bacteriologic and clinical effects. Pediatr Infect Dis J. 1987;6:458–61. DOIPubMedGoogle Scholar
- Australian Government Department of Health and Aged Care. Pertussis (whooping cough)—surveillance case definition. 2022 [cited 2023 Oct 5]. https://www.health.gov.au/resources/publications/pertussis-whooping-cough-surveillance-case-definition
- Ridda I, Yin JK, King C, Raina MacIntyre C, McIntyre P. The importance of pertussis in older adults: a growing case for reviewing vaccination strategy in the elderly. Vaccine. 2012;30:6745–52. DOIPubMedGoogle Scholar
- Bayliss J, Randhawa R, Oh KB, Kandeil W, Jenkins VA, Turriani E, et al. Perceptions of vaccine preventable diseases in Australian healthcare: focus on pertussis. Hum Vaccin Immunother. 2021;17:344–50. DOIPubMedGoogle Scholar
- Hoe Nam L, Chiu C-H, Heo JY, Ip M, Jung K-S, Menzies R, et al. The need for pertussis vaccination among older adults and high-risk groups: a perspective from advanced economies of the Asia Pacific region. Expert Rev Vaccines. 2021;20:1603–17. DOIPubMedGoogle Scholar
Figures
Tables
Cite This ArticleOriginal Publication Date: December 15, 2023
Table of Contents – Volume 30, Number 1—January 2024
| EID Search Options |
|---|
|
|
|
|
|
|



Please use the form below to submit correspondence to the authors or contact them at the following address:
Jing Chen, GSK Asia House, 23 Rochester Park, 139234, Singapore
Top